MALNUTRITION
Published on 17 Feb 2025
In India, the per capita supply of calories and protein per day is 2455 Kcal and 60 grams respectively while in China it is 12161 Kcal and 407 grams, thus indicating the disparity in the nutrition consumption in India.
Impact of Nutrient Shortage in India
✔ Malnutrition among children: A shortage of essential nutrients and vitamins can lead to malnutrition, especially among children which results in stunted growth and underweight.
● Example: As per NFHS-5, 36% of children in India are stunted and 32% are underweight.
✔ Increased disease risk: Undernourished individuals are more susceptible to infections and diseases, leading to a higher burden on the healthcare system and increased mortality rates.
● Example: The absence of vitamin A, vitamin C, vitamin E, zinc, iron etc. makes a person more prone to diseases.
Health impact on women: Lack of essential nutrients makes women more prone to anaemia and increases health risks during pregnancy and lactating phase.
● Example: As per NFHS 5, the incidence of anaemia among under-5 children has been 67% and it has been 57% among women.
✔ Educational impact: Undernourishment, especially in early childhood can negatively impact cognitive development which can lead to lower educational attainment.
● Example: Food items that aid in brain development like fatty fish, eggs, nuts, yoghurt, green vegetables etc. are not served to an undernourished child.
✔ Productivity and economic impact: Malnourished individuals may experience physical and cognitive limitations leading to reduced productivity in the workforce which hinders economic growth and development.
Challenges in Curbing Nutrient Deficit in India
✔ Limited access to nutrient-rich foods: Many individuals, particularly those in remote regions, may have limited access to a diverse and nutrient-rich diet.
● Example: Diet diversity is pretty low in the tribal areas, which has resulted in 39% of children in tribal areas being underweight (NFHS-5).
✔ Poverty and affordability concern: Poverty is a significant barrier to nutritious foods, leading to perpetuating a cycle of malnutrition, particularly among marginalized populations.
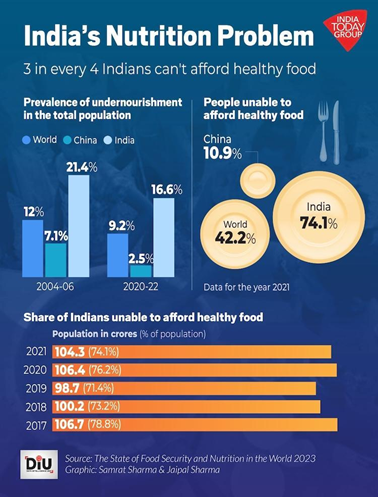
● Example: As per the FAO report, 74% of Indians cannot afford a healthy diet.
✔ Food distribution and shortage: Unequal distribution of food and inadequate storage facilities can lead to food spoilage and waste, limiting the availability of nutrient-rich foods in certain regions.
✔ Lack of nutrition education: Many people lack adequate knowledge about proper nutrition, dietary choices, breastfeeding and parenting.
● Example: Lack of awareness on the inclusion of vegetables and fruits in the diet has restricted their use to 131 kg per capita per year in India, while it is over 220 kg per capita per year in the USA.
✔ Public health infrastructure: Insufficient healthcare infrastructure and limited access to healthcare services can hinder efforts to address nutrient deficiencies, as regular check-ups and interventions are necessary to monitor and improve nutritional status.
Way Forward
✔ Nutritional awareness: Promoting nutritional awareness at the ground level is necessary by educating the public on the nutritional quality of locally available low-cost foods.
✔ Early detection of malnutrition: A well-recorded growth health chart of newborn babies and pregnant women can detect malnutrition very early.
✔ Promote breastfeeding practices: Encourage breastfeeding and create a supportive environment for breastfeeding, as it provides essential nutrients for infants and helps in preventing malnutrition.
✔ Introduce school nutrition programs: Implement and strengthen programs to provide nutritious meals to school-going children, which also promotes education participation.
✔ Implement fortification programs: Introduce food fortification programs to enhance the nutritional content of staple foods with essential vitamins and minerals.
Hence, addressing nutritional challenges is a complex and ongoing process that requires sustained efforts and a multi-stakeholder approach. The combination of policy interventions like ICDS, Poshan Abhiyaan, Mid-day meal scheme, PMMVY, etc, community engagements, education and targeted programs can contribute to improvements in nutritional outcomes in India.
COVID & Malnutrition
According to a study published in the journal Global Health Science 2020, the challenges induced by COVID-19 are expected to push another four million children into acute malnutrition. This is also evident from India's poor ranking, an abysmal 111th out of 125 countries in the latest Global Hunger Index
Impact of COVID on malnutrition in India
✔ Income loss: Economic disruptions caused by the pandemic have led to job losses, particularly those relying on daily wages, and income reductions. This increased poverty, making nutritious food less affordable.
● Example: As per the report by Azim Premji, 230 million Indians were pushed into poverty during COVID-19.
✔ Disruption of food supply chains: COVID-related restrictions disrupted food supply chains, affecting the availability and affordability of nutritious food.
● Example: During the initial weeks of COVID, the food arrivals in wholesale markets dropped by 69% and wholesale prices rose by 8%.
✔ Limited access to healthcare services: In fear of infections and overwhelmed healthcare services, including maternal and child health services results in delayed or missed opportunities for nutrition interventions, leading to worsened malnutrition.
✔ Disruption of food programmes: The closure of educational institutes where children often receive meals has disrupted essential nutrition programs.
● Example: During the peak of COVID, around 116 million children were losing out on school meals.
✔ Impact on women: Lack of vital nutrients deteriorated the health of pregnant women, who had limited access to institutional care and proper food supplements during COVID-19.
● Example: Around 20% decline in institutional delivery was witnessed during COVID.
✔ Healthcare prioritization: The focus of COVID has diverted resources from existing health programs, which led to neglect of preventive care and treatment measures for malnutrition.
Government initiatives to address malnutrition during COVID
✔ PM Garib Kalyan Anna Yojana: A food security program to ensure food and nutrition security during the pandemic.
✔ Cash transfer programme: 30000 crore was transferred into the account of woman Jan Dhan Account holders and over 5000 crore into linked LPG connections.
✔ Cash component of the Mid-day meal programme: The Centre decided to transfer its share of the cooking cost components of the mid-day meal scheme to the bank accounts of beneficiaries.
Though there was a setback in addressing malnutrition during the initial phase of the pandemic, the government responded actively to address the health, income and nutrition shortage through efficient public spending.